First of all,
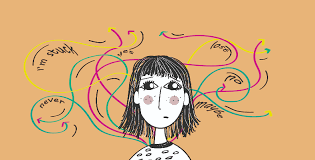
While depression and attention deficit hyperactivity disorder (ADHD) are two different mental health problems, they frequently coexist and pose serious difficulties for those who suffer from both. While impulsivity, hyperactivity, and inattention are the hallmarks of ADHD, depression is marked by enduring emotions of melancholy, hopelessness, and disinterest in activities. When these disorders coexist, it can worsen symptoms and have a major influence on day-to-day functioning. But despite their impact and frequency, there is still stigma associated with depression and ADHD, which prevents people from getting the help and knowledge they so sorely need.
Knowing Depression and ADHD:
The symptoms of ADHD, a neurodevelopmental condition that affects people of all ages, frequently start in childhood and continue throughout maturity. Worldwide, the prevalence of ADHD is thought to be between 5 and 7% of children and adolescents, while 2.5% of adults still exhibit symptoms. Although the precise origin of ADHD is unknown, environmental and genetic factors are thought to be involved.
In contrast, depression is a type of mood disorder marked by enduring emotions of hopelessness, worthlessness, and misery. It is a major contributor to disability globally, affecting about 264 million people. Similar to ADHD, depression can strike at any age and is influenced by a number of variables, such as experiences in life, brain chemistry, and heredity.
The Confluence of Depression and ADHD:
Studies show that there is a strong correlation between depression and ADHD, with those who have been diagnosed with ADHD having a higher chance of acquiring depression than the general population. Depression can start and worsen as a result of ADHD symptoms such impulsivity, difficulty concentrating, and low self-esteem. Similarly, the difficulties linked to depression, such exhaustion, poor memory, and low motivation, can resemble or exacerbate symptoms of ADHD, creating a complex interaction between the two disorders.
Dispelling the Myth:
Despite the fact that depression and ADHD are common and have significant effects, the stigma associated with mental illness endures, keeping many people from getting the care and assistance they require. Misconceptions, preconceptions, and cultural attitudes that support discrimination, shame, and isolation are the root causes of stigma. When it comes to ADHD, misunderstandings regarding the disorder’s cause being indifference or lack of self-control can make those who are impacted feel inadequate and guilty of themselves. Similarly, depression is not acknowledged as a real medical problem that needs to be treated, but rather is stigmatized as a sign of weakness or a character flaw.
Education, knowledge, and candid communication are necessary to dispel the stigma associated with depression and ADHD. By busting misconceptions and giving truthful information about these illnesses, we can promote compassion and empathy. It is crucial to stress that biological, psychological, and environmental variables have a medical role in ADHD and depression; these disorders are not caused by moral flaws or personal shortcomings.
Looking for Assistance:
The fear of rejection or criticism is a major obstacle to getting help for depression and ADHD. Many people may be reluctant to share their challenges for fear of being mislabeled or misinterpreted. But seeking assistance is an essential first step in controlling symptoms and enhancing quality of life.
Support for depression and ADHD can be obtained through a variety of channels, such as counseling, medication, support groups, and self-help techniques. A popular method that can assist people in improving self-esteem, coping skills, and challenging negative thought patterns is cognitive-behavioral therapy, or CBT. To reduce symptoms and improve functioning, doctors may prescribe stimulants, antidepressants, or a mix of the two. Peer networks and support groups also give people a feeling of validation and belonging, enabling them to talk about their experiences and gain knowledge from others going through comparable difficulties.
It is critical to stress that there is no one-size-fits-all approach to treating ADHD and depression; rather, a customized combination of therapies may be needed depending on the needs of the patient. Working together with medical specialists, such as psychologists, counselors, and psychiatrists, can assist people in creating individualized treatment programs and gaining access to the resources required for rehabilitation.
In summary:
Although depression and ADHD are serious mental health illnesses that can have a substantial impact on a person’s life, the stigma associated with them frequently keeps people from getting the help they require. We can make the environment more welcoming and encouraging for people with ADHD and depression by dispelling the stigma through awareness-raising, education, and candid communication. It’s critical to motivate people to seek help—through counseling, medicine, or support groups—in order to manage their symptoms and enhance their general wellbeing. When we work together, we can fight stigma, advance understanding, and give people the tools they need to overcome mental health obstacles and lead happy, productive lives.